Patient Information
Few Facts about Liver
- Liver is the only organ in the body which can regenerate itself
- Up to 70% of liver can be removed safely from a donor
- Liver grows back to its full size in a few weeks
- Liver transplantation is the only cure for advanced stages of cirrhosis
- Liver can be donated by a brain dead person or by a close relative with matching blood group
- Liver transplantation, if done in time, has over 90% success rate
- After liver transplantation, life can be completely normal but close follow up is essential
Who Needs a Liver Transplant?
Liver has a large reserve of function and it is not until more than 80% of functional liver cells have died due to various diseases that signs and symptoms of liver failure begin to appear. Such diseases may ultimately overwhelm the inherent capacity of liver to recover from injury and the liver fails. In such conditions, liver transplantation offers not only the realistic hope of survival but also the possibility of cure. Liver failure may develop either suddenly (acute) or slowly (chronic).
 Acute or Fulminant Liver Failure may develop commonly due to infections with viruses (Hepatitis A, E) or Drugs (drugs for tuberculosis, high doses of paracetamol) intake. Such a liver failure develops suddenly (in matter of hours to days), progresses very rapidly often leading to death due to swelling of the brain or failure of other vital organs. A timely liver transplantation offers the only realistic hope of survival in these patients.
Acute or Fulminant Liver Failure may develop commonly due to infections with viruses (Hepatitis A, E) or Drugs (drugs for tuberculosis, high doses of paracetamol) intake. Such a liver failure develops suddenly (in matter of hours to days), progresses very rapidly often leading to death due to swelling of the brain or failure of other vital organs. A timely liver transplantation offers the only realistic hope of survival in these patients.
 Chronic liver failure (cirrhosis), on the other hand, develops slowly (over a period of months) and is a result of continuing slow damage to the liver. Common causes of such slow damage of liver include viral infections (Hepatitis B or C), regular intake of alcohol etc. Signs that the liver is beginning to fail include jaundice, excessive tiredness, ascites (accumulation of fluid in the tummy), encephalopathy (drowsiness and confusion), vomiting of blood rupture of distended veins into the food-pipe and effects of liver disease on other vital organs like kidneys, lungs etc. leading to their dysfunction.
Chronic liver failure (cirrhosis), on the other hand, develops slowly (over a period of months) and is a result of continuing slow damage to the liver. Common causes of such slow damage of liver include viral infections (Hepatitis B or C), regular intake of alcohol etc. Signs that the liver is beginning to fail include jaundice, excessive tiredness, ascites (accumulation of fluid in the tummy), encephalopathy (drowsiness and confusion), vomiting of blood rupture of distended veins into the food-pipe and effects of liver disease on other vital organs like kidneys, lungs etc. leading to their dysfunction.
Some patients with liver cancer are also candidates for liver transplant. Cancer often develops in those who have cirrhosis already and extensive surgery to remove the tumor is not possible in such cases. Besides, there are genetic disorders which affect the liver and result in liver disease such as Criggler-Najjar Syndrome or Progressive Familial Intra-hepatic Cholestasis which might need liver transplantation. Finally, there are also genetic disorders which do not cause liver disease but are cured by a liver transplant such as Primary Hyperoxaluria, Familial Amyloid Polyneuropathy, Maple Syrup Urine Disease etc.
Donor
Living Donor Liver Transplant
Like Japan and Korea, majority of liver transplants in India have been from living donors from the patient's family. Such a liver donor is a family member of the patient who volunteers to have an operation to have a portion of his/ her liver removed for transplantation into the patient. Liver has a large reserve of function and a remarkable ability to recover from injury. This means that up to 70% of normal healthy liver can be removed safely and the remaining liver will function and grow to the size of a normal liver. 90% of this growth happens in 2-3 months although slow growth occurs after that as well. The liver function tests (LFT) typically return to normal in 5-7 days. Ideally, the donor must be between the ages of 18 and 60, have a blood group compatible with that of the patient and be healthy and fit for surgery. Overweight people and those who consume alcohol regularly are usually not suitable.
The amount of liver removed from the donor depends on the weight of the patient and the size and anatomy of the liver. As a general rule, the weight of liver required for transplant is 0.8% of the weight of the patient. This means a 70 kg patient requires at least 560 g of liver to be transplanted.
Like anyone undergoing abdominal surgery, the donor should avoid lifting heavy weights for 3 months. After that there is no restriction on activity.
Deceased (Cadaveric) Donor Liver Transplant
Deceased (Cadaveric) donor is a person who is declared ‘brain-dead’ but who can donate other organs of his body as the blood supply to these organs is maintained. The organs of such a ‘brain-dead’ person can be used for transplantation if the next-of-kin give consent. Donor should be blood group compatible. Unfortunately, due to various socio-cultural factors, this form of organ donation is rare in India and the chances of getting such an organ in time are poor for a sick patient.
Living Donor Guidelines
As per the Transplantation of Human Organs Act (THOA) of India, The Living Donor has to fulfill certain mandatory requirements for the approval by the competent authority (Authorization Committee). Hence it is recommended to go through the following forms and annexure to ensure that the patient and donor fulfils all the legal requirements and carries the necessary documentation so that time is not lost unnecessarily once the patient reaches Delhi. The patient may contact the Transplant Team in case of any queries.
Annexure I: Preliminary Donor Workup for Liver Transplant
Annexure II: Documents Required For Legal Workup for Liver Transplantation
Annexure III: Liver Donation Forms & Affidavit Formats
Transplant Process
For your Liver Transplantation journey, the transplant process is essentially divided into four stages to guide you along the way.
Initial contact:
1. The patient or family can contact us by e-mail or phone and send all the patient's relevant medical records by e-mail or fax or courier.
Mobile: +91-9811765618
E-mail: drsanjaynegi@gmail.com
2. After reviewing the medical details, we will revert with our opinion and course of treatment including need for liver transplantation, financial details and donor requirements that are relevant to the case.
Pre-transplant evaluation (Liver Transplant Assessment)
This stage begins when the patient arrives at the hospital and begins the process of medical evaluation, orientation, informed consent, and other preliminary activities. Patient undergoes an evaluation for the cause of end-stage liver disease and for the fitness for a major surgery like liver transplantation. As end stage liver disease has adverse effects on other organs of the body, a multidisciplinary team consisting of Transplant surgeons, Anesthesiologist, Hepatologist, Cardiologist, Chest physician, Dental surgeon, Psychiatrist. Recipient evaluation is done in three phases and typically takes 5-7 days in hospital.
Phase 1: To establish the cause of liver disease, determine the severity of liver disease and assess the urgency of the transplant.
Phase 2: To determine the fitness of the patient for a transplant. Vital organs such as heart, lungs, kidneys, blood counts are tested and the presence of any infection is ruled out. Sometimes the patient is often very sick before a liver transplant or if the tests detect any abnormality in the functioning of organ system or infection then the patient’s condition needs to be medically improved to the point where a transplant can safely be done. This comprises chiefly of identifying and treating any infection and making sure that the other organs (particularly the kidneys which tend to be affected by the liver disease or the medicines used to treat it) are working well.
Phase 3: The final phase consists of psychological and mental preparation of the patient. The patient and the family are counseled about the procedure, hospital stay, the likely course after surgery, follow up and aftercare.
The further preparation is dependent on the fact whether the patent has a willing and blood group matched family donor available. If there is a willing and blood group matched family donor available, he/she is evaluated for donation and a transplant is scheduled or else the patient is placed on the waiting list for deceased organ (cadaveric) donation.
Living Related Donation: Once a willing family donor has been identified, he/she is subjected to detailed evaluation to assess the health, size and make of liver as well as general fitness of donor for surgery. Ideally, the donor must be between the ages of 18 and 60, have a blood group compatible with that of the patient and be healthy and fit for surgery. Overweight people and those who consume alcohol regularly are usually not suitable (Annexure I). Such detailed assessment helps in proper selection of the donors so that the risk to the donor is minimal. The risk to the donor from the operation is 0.1-0.5% depending on how much of the liver needs to be removed. Once the donor has been deemed suitable for donation based on the results of such evaluation, the donor would need to submit certain Documents (Annexure II & Annexure III) to facilitate the Legal Clearance from Authorization Committee. The transplant surgery may be scheduled anytime once clearance is obtained from Authorization Committee. This step normally takes about 3-5 days but in the case of an emergency clearance can be obtained within 1-2 days.
Cadaveric (Deceased) Donation: If the patient does not have a willing family donor, he/she is put on the waiting list for deceased organ (cadaveric) donation. While on such a waiting list, the patient follows up with the Transplant Team until a suitable liver becomes available. The waiting time apart from the availability of organ (shortage of donors), depends on the general medical condition of the patient. Thousands of people die each year while waiting for a cadaveric liver to be offered. Organ donation after ‘brain-death’ is still evolving in India but it is slowly and steadily making a place in the transplant program. Once the transplant team gets information regarding organ availability, the recipient on the waiting list for cadaveric liver transplant is contacted and admitted to the hospital. Simultaneously the retrieval team gets involved in the organ procurement while the patient is taken up for the surgery. Liver once retrieved is transported to the recipient hospital in a cold preservative solution and transplanted in the patient.
Operation: The operation involves removal of the diseased liver and replacing it with a healthy liver. This is a complex and highly technical operation where the new liver with the conduits (arteries, veins and bile duct) are joined to the corresponding structures in the patient. The operation typically takes around 8-10 hours in a cadaveric and 10-12 hours in a living related liver transplantation.
Post-transplant care: The patient usually stays in hospital for 2-3 weeks depending on the pre-transplant condition and his/her recovery. After surgery patient is started on medications (immunosuppressants) to prevent the patient’s own body reacting to the new liver and rejecting it. However, these medicines make the patient susceptible to infection and the patient is also given prophylactic antibiotics and anti-fungals and sometimes anti-virals as well. Over a period of time the requirement of these medicines comes down and they are gradually withdrawn. At least one immunosuppressant medicine continues lifelong in a small dose. After transplantation patients have a good quality of life and most of them lead a comfortable and healthy life. For donor, the life is otherwise normal; there are no medicines in the long term and no dietary restrictions. Like anyone undergoing abdominal surgery, the donor should avoid lifting heavy weights for 3 months.
Transplant Procedure
The liver transplant operation involves removal of the unhealthy liver of the patient and replacing it with the healthy liver. The operation to remove the diseased liver of the patient (recipient hepatectomy) is technically challenging because the liver is firmly attached to surrounding organs with tissues containing many thin walled blood vessels (collaterals) with blood under a lot of pressure (portal hypertension). A lot of bleeding can occur during this phase of surgery and enough blood should be arranged to replace the losses. The entire diseased liver must be removed in such a way that the main blood vessels and bile duct of the patient are preserved to be joined to those of the new liver.
In living donor operation, the donor liver must be divided into two parts in such a way that not only the part which is left behind should be sufficient & working well in the donor but also the part of liver which is to be removed should be sufficient for the patient and work well after implantation. Both parts of the liver must have a blood supply into the liver as well as a way for the blood to leave the liver and a way for the bile to flow out of the liver. This is a much more difficult and challenging operation than removal of a portion of the liver for disease or cancer. In deceased (cadaveric) donor operation whole liver is removed.
Once removed, the donor liver (whole or portion of liver) is flushed with cold preservative solution and the blood vessels are prepared to be connected with those of the patient. This often involves extending the vessels of the donor liver with segments of vessels taken from the patients removed liver. The new liver is then implanted into the patient and all the blood vessels and the bile ducts joined to their counterparts in the patient. A Doppler ultrasound check is performed on the operation table to confirm that all the blood vessels are working well.
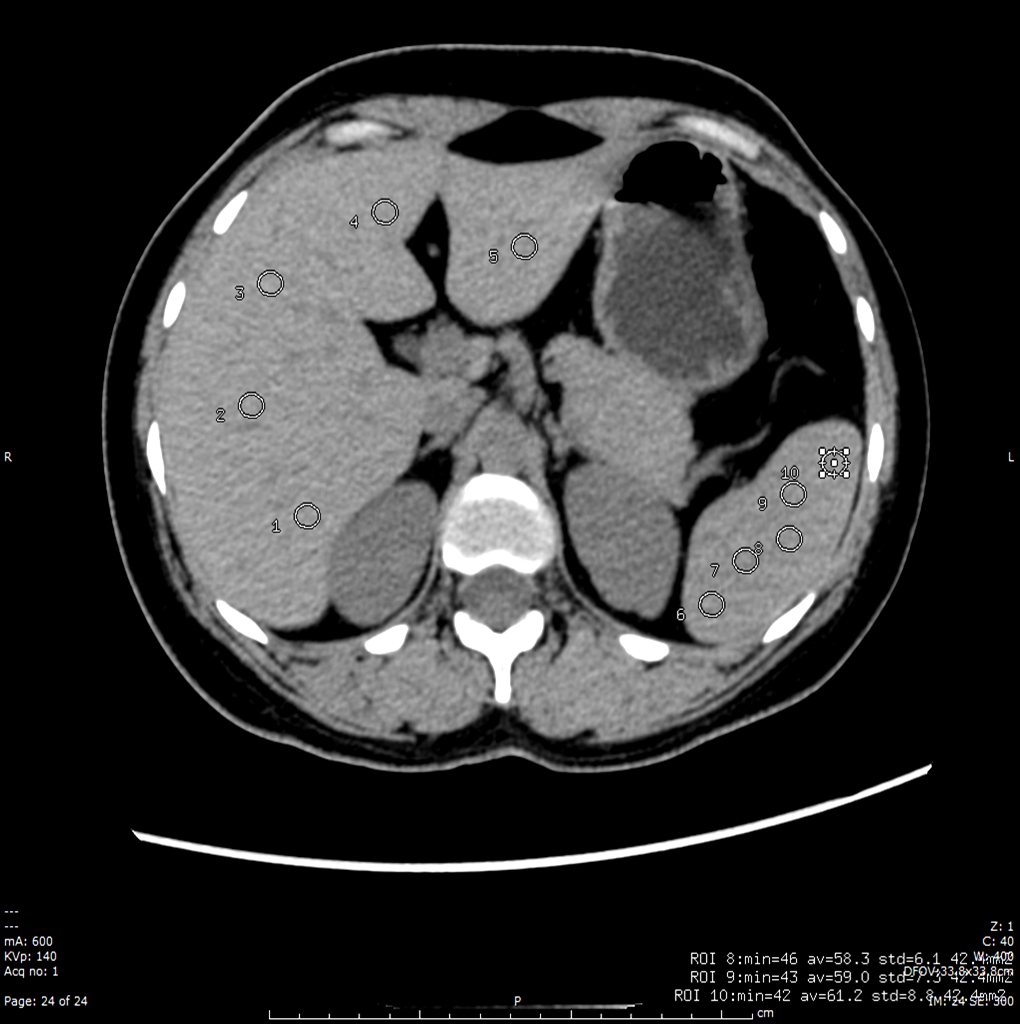
 Plain CT scan of Donor is done to assess amount of fat in liver
Plain CT scan of Donor is done to assess amount of fat in liver
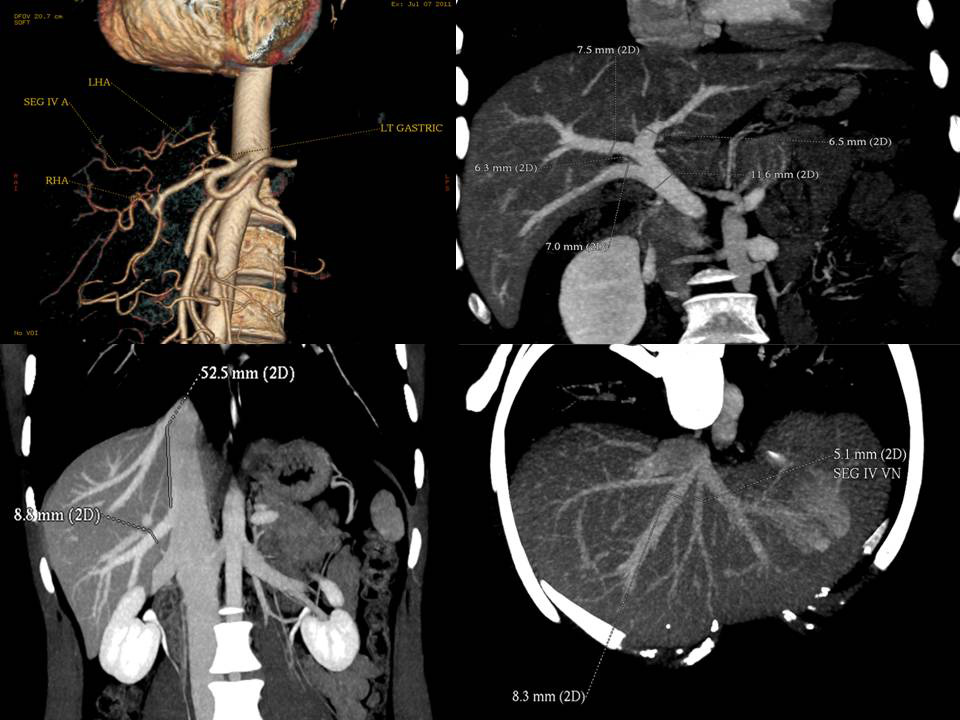 CT Angiogram of Donor gives detailed information about blood vessels in the donor and helps plan the operation.
CT Angiogram of Donor gives detailed information about blood vessels in the donor and helps plan the operation.
 MRCP of Donor gives us detailed idea about the anatomy of Bile ducts
MRCP of Donor gives us detailed idea about the anatomy of Bile ducts
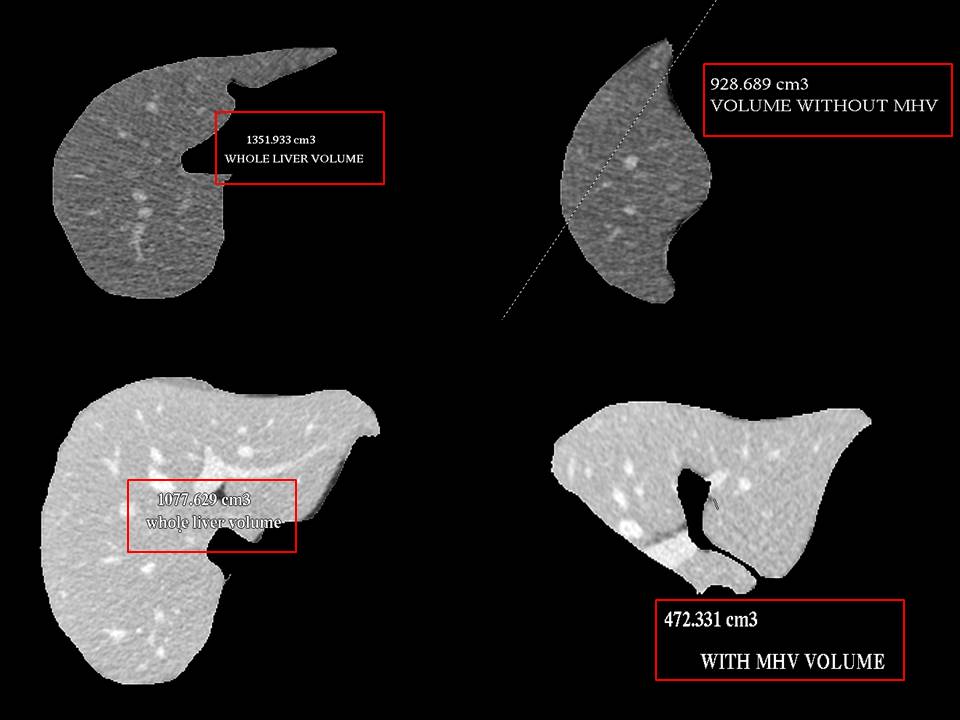
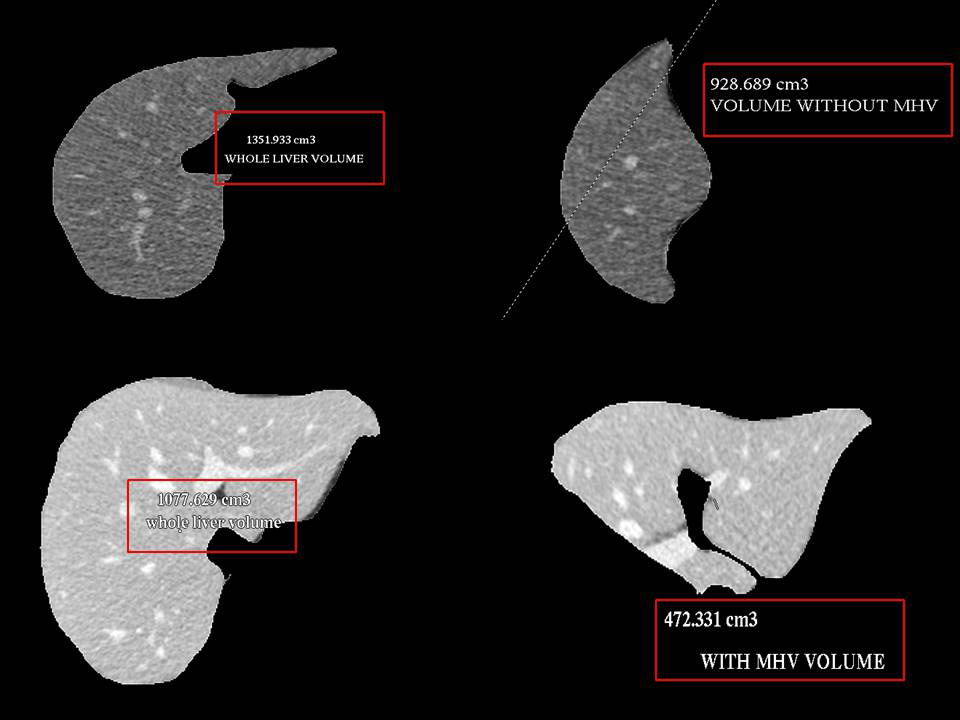 Volumetry of Donor Liver using CT scan gives an idea about the volumes of each side of liver
Volumetry of Donor Liver using CT scan gives an idea about the volumes of each side of liver
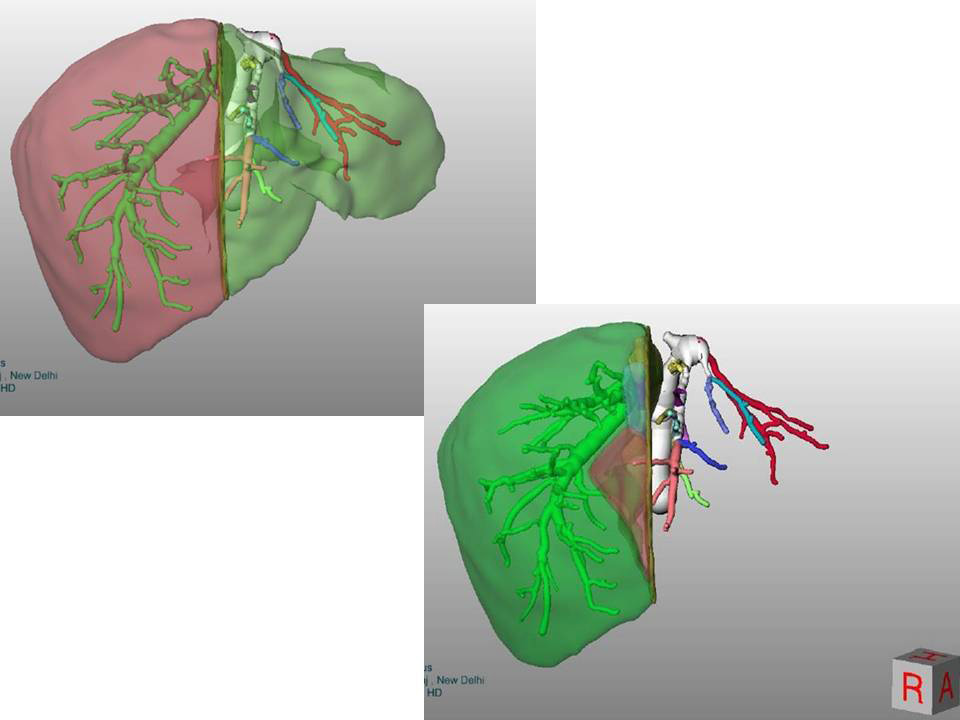 In complex cases sophosticated software helps in pre-surgery planning and virtual surgery
In complex cases sophosticated software helps in pre-surgery planning and virtual surgery
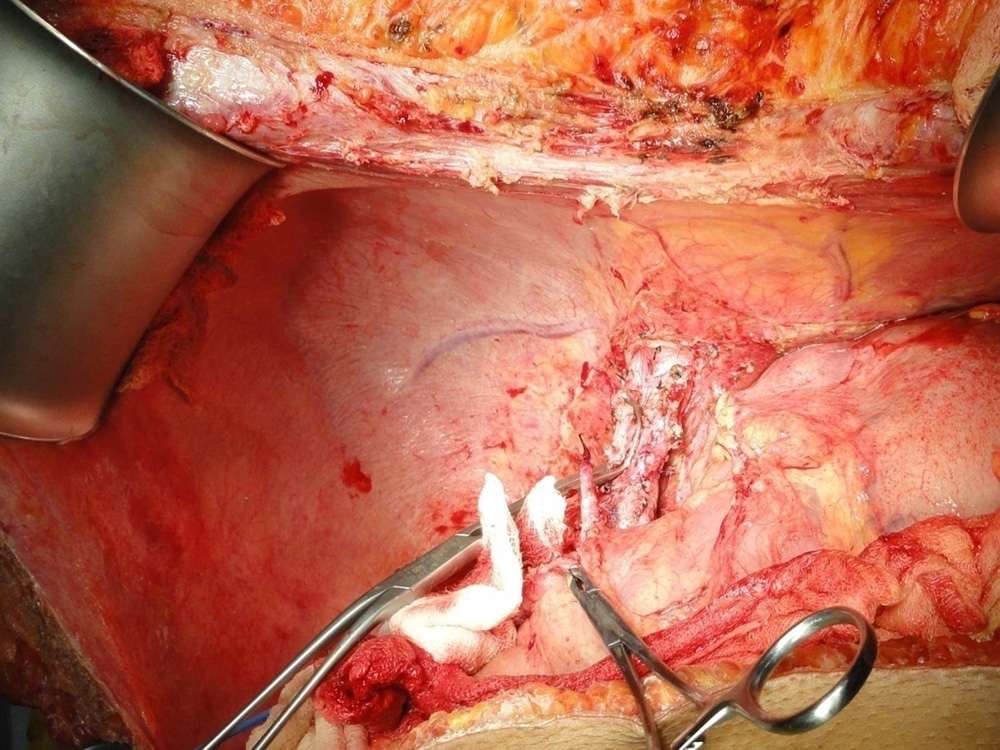
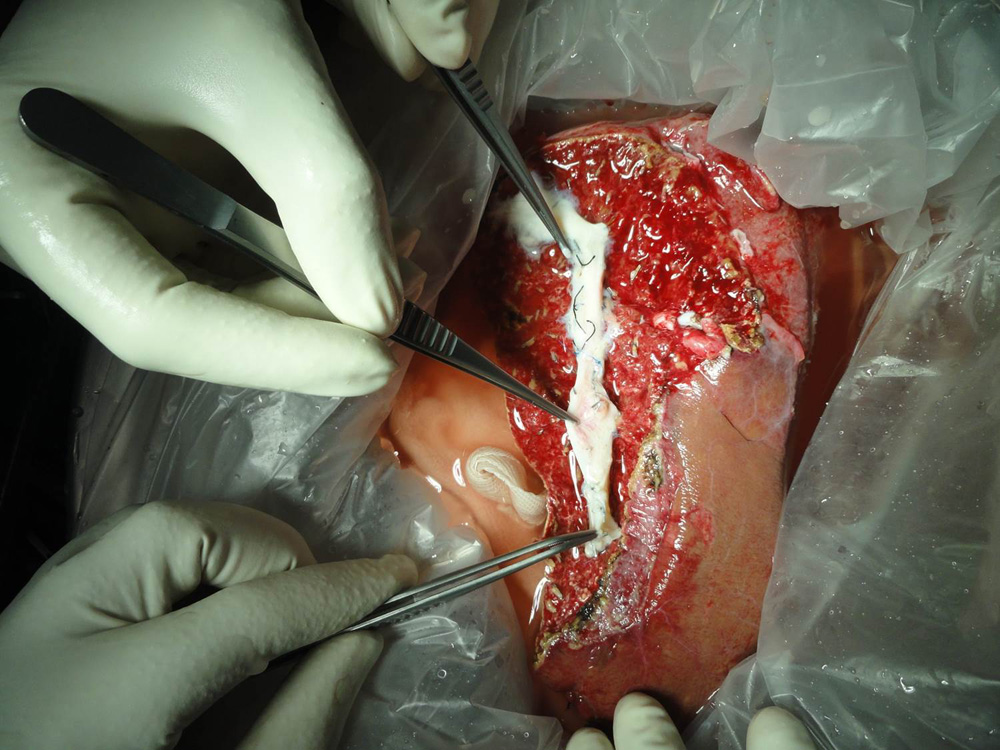
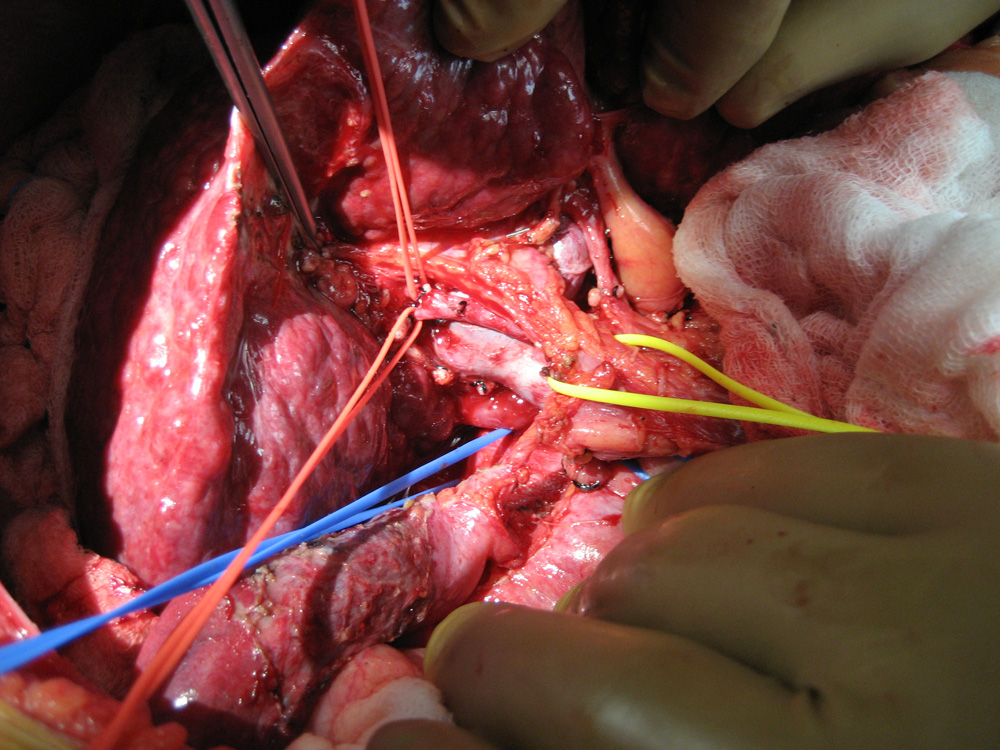 Blood vessels and bile duct of patient's liver being dissected
Blood vessels and bile duct of patient's liver being dissected
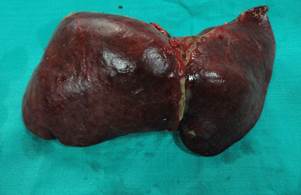
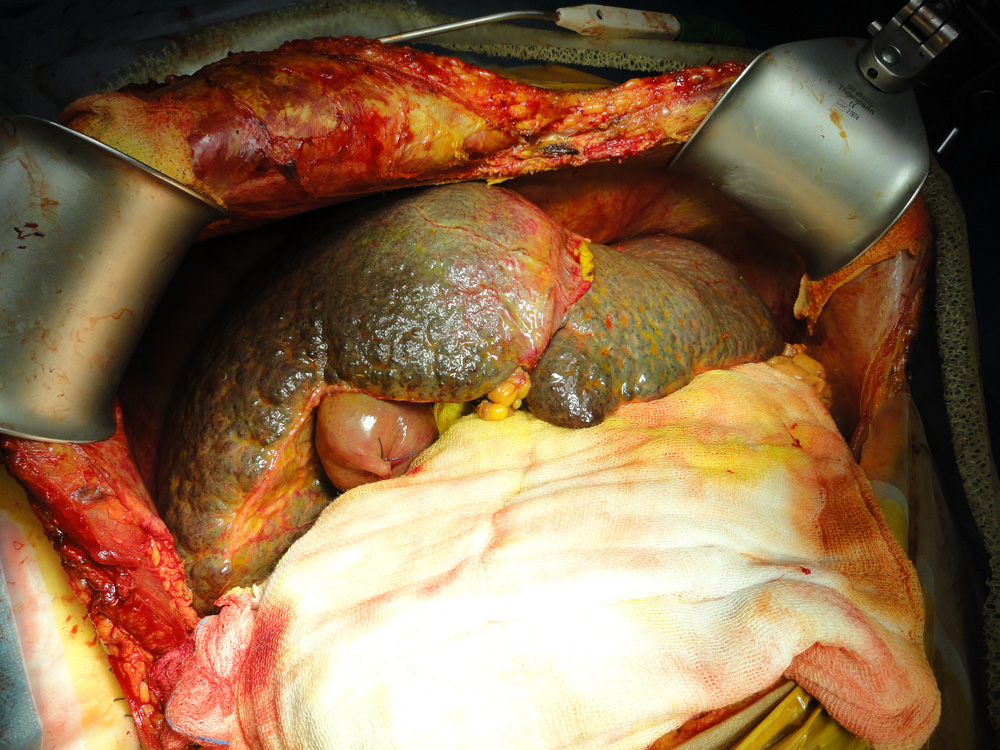 Diseased liver of the patient afflicted with Cirrhosis
Diseased liver of the patient afflicted with Cirrhosis
 Diseased liver of the patient has been removed preseving blood vessels and bile duct
Diseased liver of the patient has been removed preseving blood vessels and bile duct
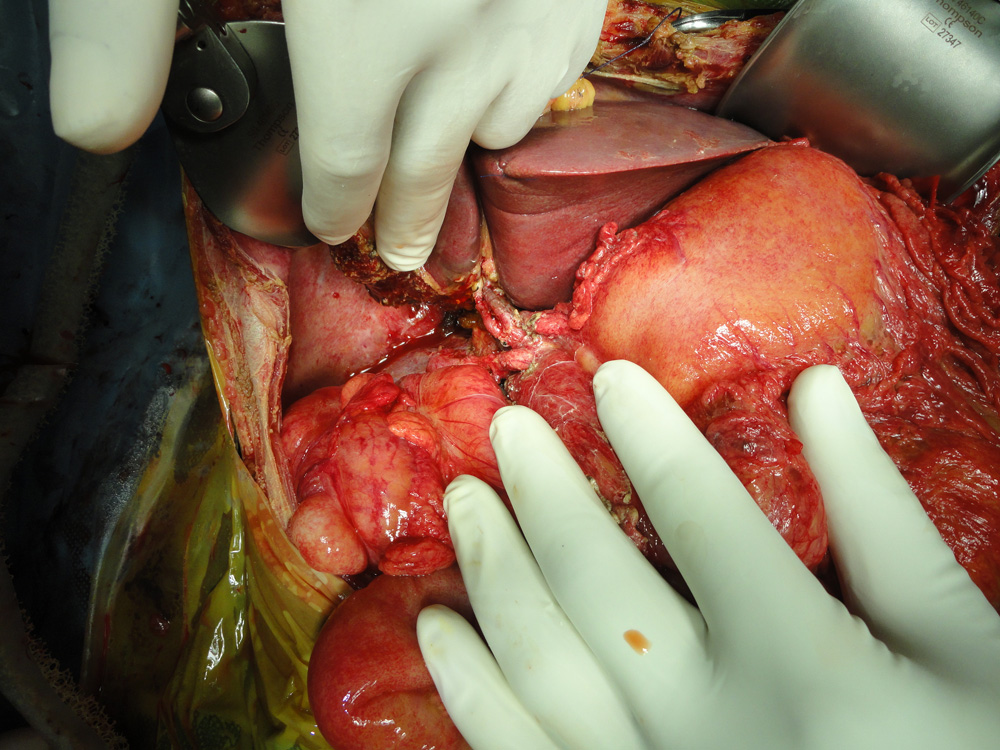
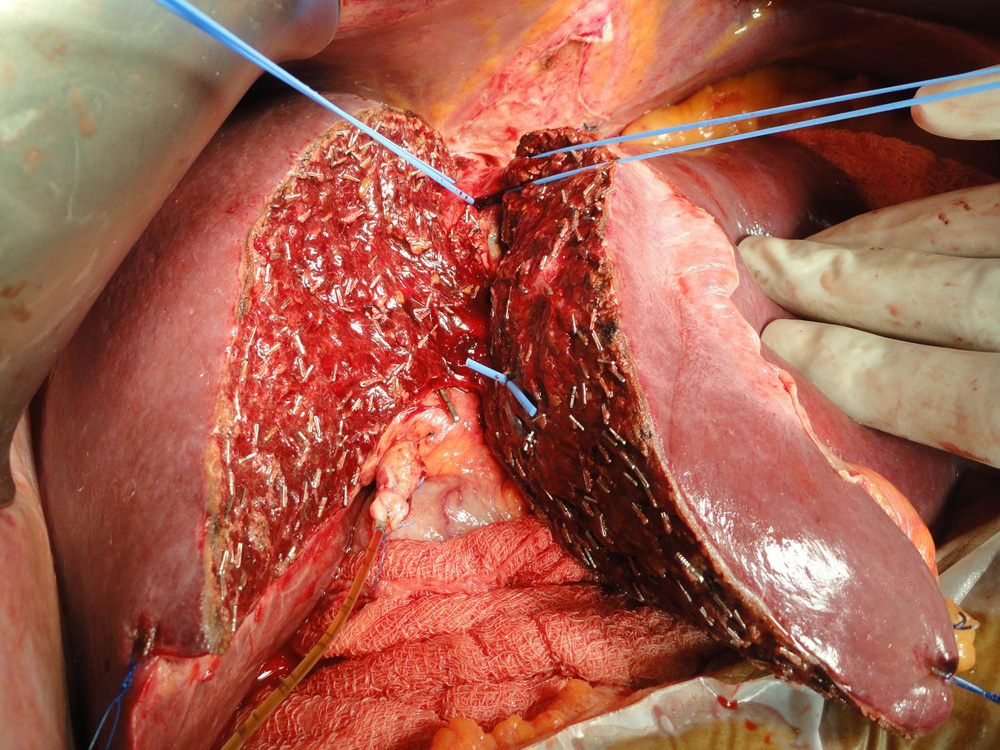 Donor liver is being split taking great care to preserve blood supply to both sides of the liver.
Donor liver is being split taking great care to preserve blood supply to both sides of the liver.
 The portion of the donor liver which is going to be transplanted (in this case right lobe) is seen here
The portion of the donor liver which is going to be transplanted (in this case right lobe) is seen here
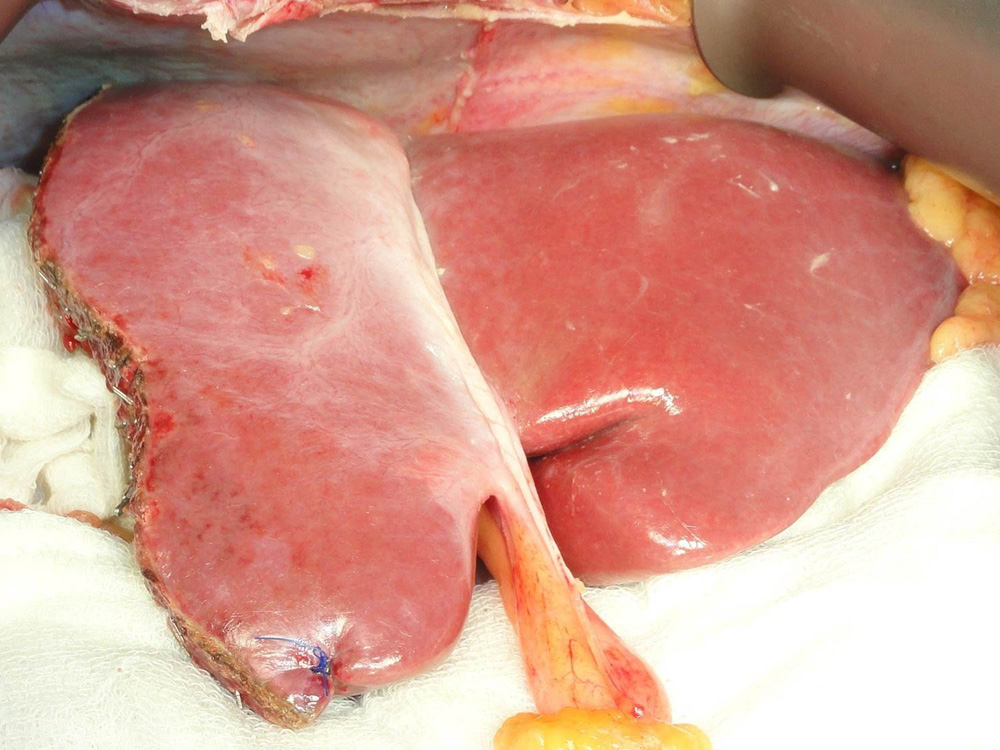 The remaining donor liver is seen after the portion to be transplanted has been removed.
The remaining donor liver is seen after the portion to be transplanted has been removed.
 The liver graft being modified during bench procedure
The liver graft being modified during bench procedure
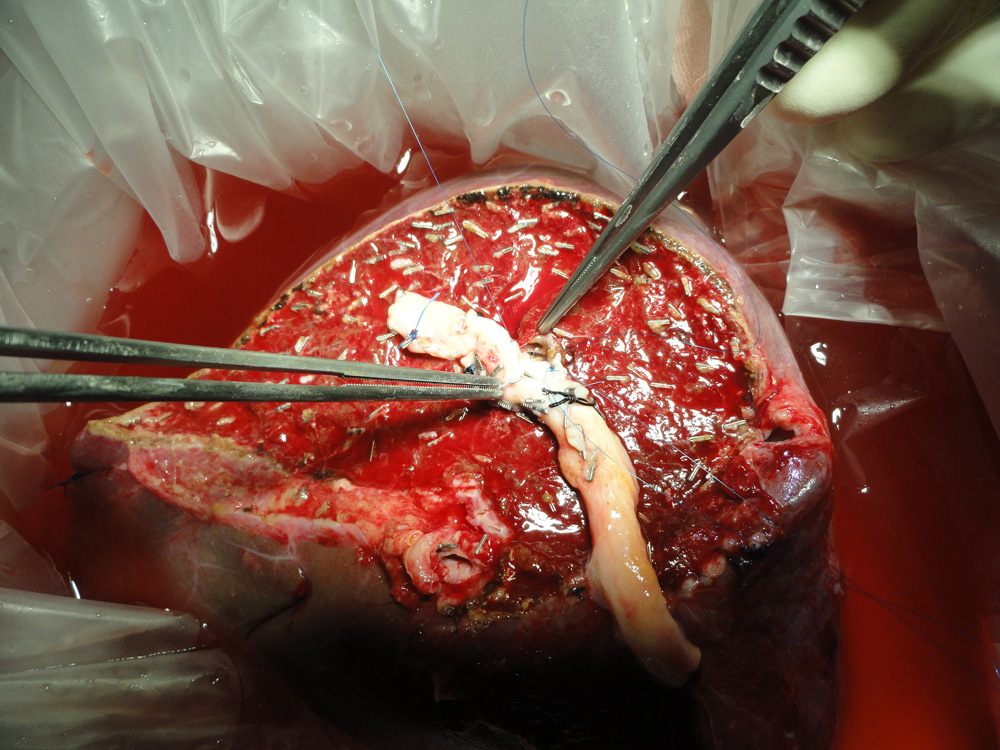
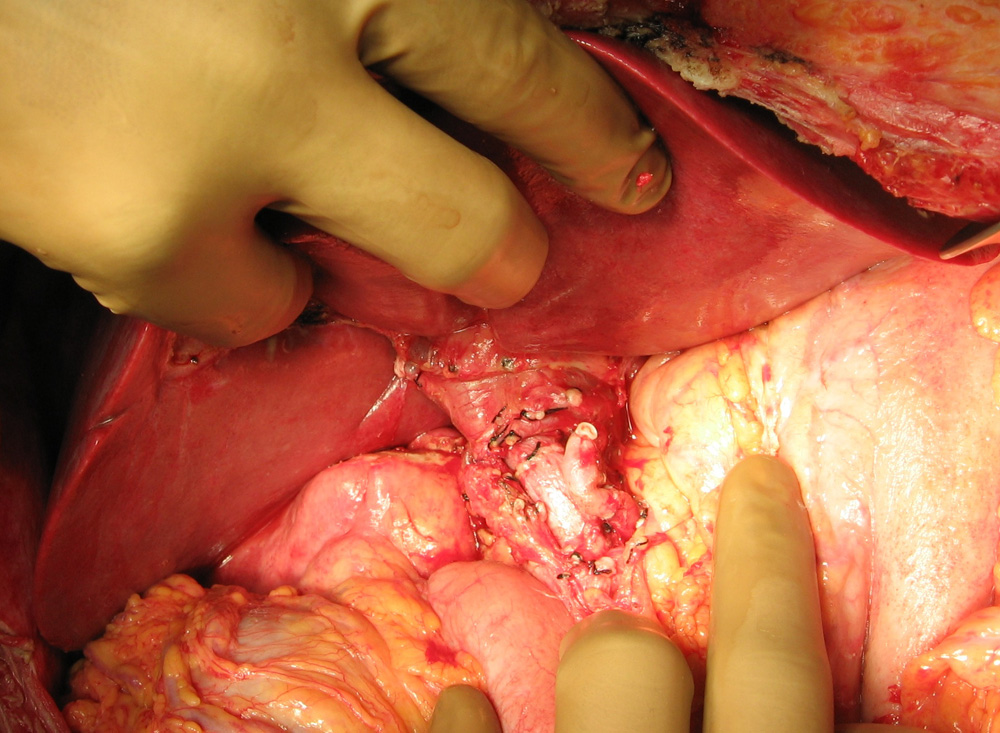
 The middle hepatic vein is being reconstructed with a vein graft taken from the patient’s removed liver
The middle hepatic vein is being reconstructed with a vein graft taken from the patient’s removed liver
 Left lobe liver transplant in a child. Two arteries have been reconstructed
Left lobe liver transplant in a child. Two arteries have been reconstructed
 Deceased donor (Cadaver) graft after retrieval
Deceased donor (Cadaver) graft after retrieval
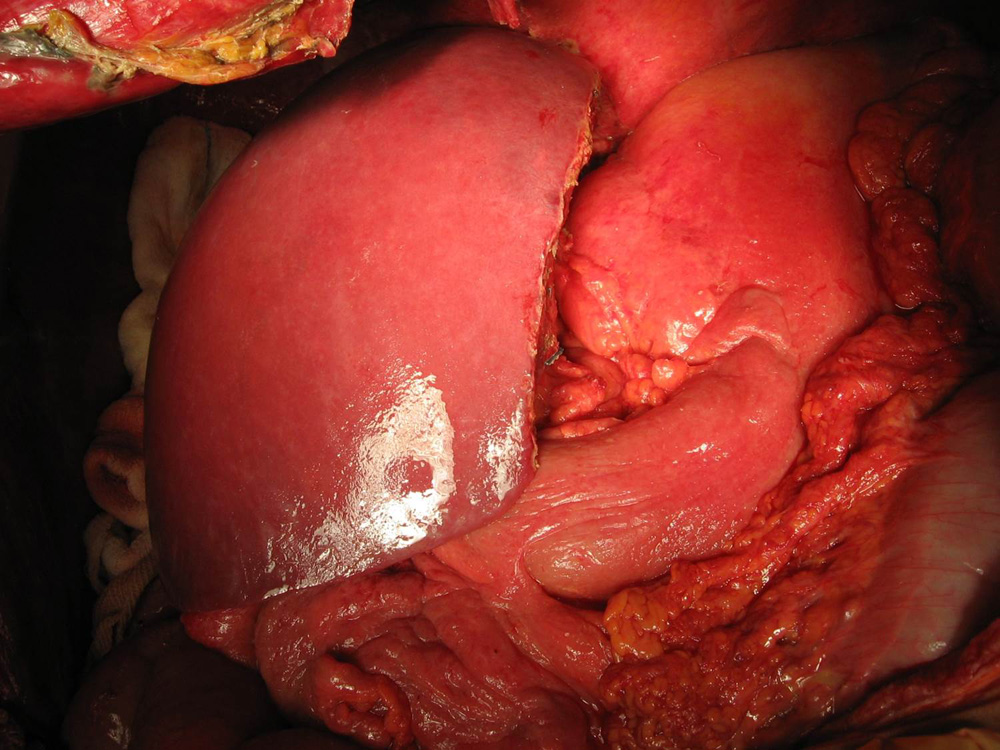
 Deceased donor (Cadaver) graft after reperfusion
Deceased donor (Cadaver) graft after reperfusion
 Blood flow in the transplanted liver being verified using Doppler Ultrasound
Blood flow in the transplanted liver being verified using Doppler Ultrasound
 New Right-sided Liver at the completion of operation
New Right-sided Liver at the completion of operation
